| Therapy | Type | Indications | Key Side Effects | Key Considerations |
|---|---|---|---|---|
| BCG | Immunotherapy | High-risk NMIBC (CIS, high-grade Ta/T1) | Dysuria, frequency, hematuria, fever, fatigue, rare sepsis | Gold standard; requires induction + maintenance; shortages common |
| Mitomycin C (MMC) | Chemotherapy | Intermediate- to high-risk; post-TURBT | Chemical cystitis, rash, bladder irritation | Often used post-TURBT (within 24 hrs); some use for maintenance |
| Gemcitabine | Chemotherapy | BCG-unresponsive or intermediate-risk NMIBC | Mild bladder symptoms (dysuria, frequency) | Good safety profile; increasing use in BCG failure or shortage |
| Gemcitabine + Docetaxel | Chemotherapy (Combo) | BCG-unresponsive or relapsing disease | Mild urinary symptoms, rare systemic effects | Effective salvage regimen; growing role in BCG-unresponsive cases |
| Adstiladrin (nadofaragene firadenovec) | Gene Therapy | BCG-unresponsive CIS ± Ta/T1 | Fatigue, urgency, dysuria, hematuria | FDA-approved gene therapy; instilled every 3 months; IFNα gene-based |
| Anktiva (N-803) | Immunotherapy | BCG-unresponsive CIS ± papillary tumors (with BCG) | Fatigue, flu-like symptoms, urinary urgency | FDA-approved with BCG; IL-15 superagonist; promising results in BCG-unresponsive disease |
| UGN-102 (mitomycin gel) | Chemotherapy | Low-grade intermediate-risk NMIBC | Urinary frequency, dysuria, hematuria, bladder spasms | Thermo-sensitive gel; prolongs drug contact time; promising in low-grade tumors |
| TAR-200 (gemcitabine implant) | Chemotherapy delivery system | BCG-unresponsive NMIBC | Urinary tract irritation, dysuria, urinary retention | Implant releasing gemcitabine over weeks; alternative delivery approach |
Regular cystoscopy, urine tests, and imaging to monitor for recurrence.
| Risk Category | Cystoscopy | Urine Cytology | Imaging (Upper Tract) | Other Notes |
|---|---|---|---|---|
| Low-Risk | Every 3 months for 6–12 months, then annually | Optional | Only if indicated (e.g., hematuria) | May stop after 5 years if no recurrence |
| Intermediate-Risk | Every 3 months for 2 years, every 6 months to 5 years, then annually | At each visit | Every 1–2 years or as needed | Consider single-dose intravesical chemo post-TURBT |
| High-Risk | Every 3 months for 2 years, every 6 months until year 5, then annually | At each visit | Annually (CT urogram or ultrasound + cytology) | Consider repeat TURBT, BCG maintenance, or early cystectomy |
| Risk Group | 1-Year Recurrence Risk | 5-Year Recurrence Risk | 1-Year Progression Risk | 5-Year Progression Risk | Common Characteristics |
|---|---|---|---|---|---|
| Low Risk | 15% | 31% | <1% | ~1% | Small, single, low-grade Ta tumor, no CIS |
| Intermediate Risk | 24–38% | 38–62% | 1–5% | 6–17% | Multiple or recurrent low-grade tumors, no CIS |
| High Risk | ~61% | ~78% | ~17% | >45% | High-grade T1, CIS, large/multiple tumors |
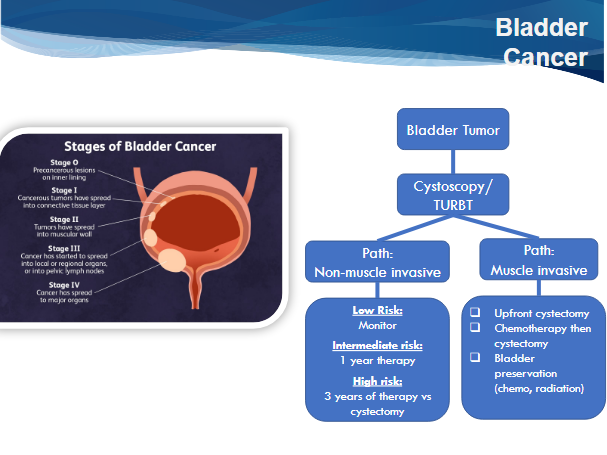
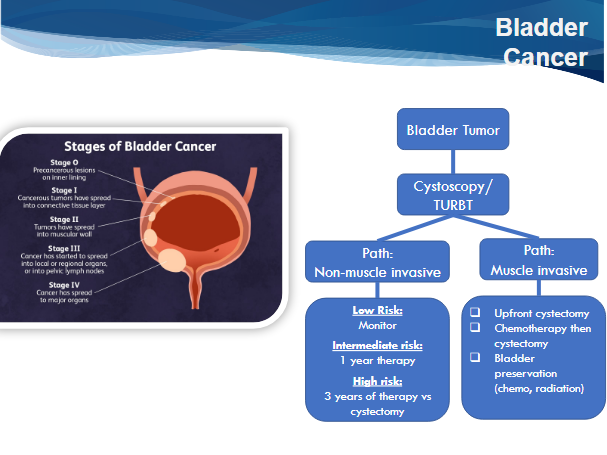
Non-Muscle Invasive Bladder Cancer (NMIBC) refers to bladder cancers that are confined to the inner layers of the bladder wall and have not spread to the muscle layer. These cancers account for approximately 75% of newly diagnosed bladder cancer cases.
Contact us if you experience any of these symptoms.
NMIBC is diagnosed using the following methods:
Endoscopic removal of visible tumors from the bladder lining.
Drugs delivered directly into the bladder:
| Therapy | Type | Indications | Key Side Effects | Key Considerations |
|---|---|---|---|---|
| BCG | Immunotherapy | High-risk NMIBC (CIS, high-grade Ta/T1) | Dysuria, frequency, hematuria, fever, fatigue, rare sepsis | Gold standard; requires induction + maintenance; shortages common |
| Mitomycin C (MMC) | Chemotherapy | Intermediate- to high-risk; post-TURBT | Chemical cystitis, rash, bladder irritation | Often used post-TURBT (within 24 hrs); some use for maintenance |
| Gemcitabine | Chemotherapy | BCG-unresponsive or intermediate-risk NMIBC | Mild bladder symptoms (dysuria, frequency) | Good safety profile; increasing use in BCG failure or shortage |
| Gemcitabine + Docetaxel | Chemotherapy (Combo) | BCG-unresponsive or relapsing disease | Mild urinary symptoms, rare systemic effects | Effective salvage regimen; growing role in BCG-unresponsive cases |
| Adstiladrin (nadofaragene firadenovec) | Gene Therapy | BCG-unresponsive CIS ± Ta/T1 | Fatigue, urgency, dysuria, hematuria | FDA-approved gene therapy; instilled every 3 months; IFNα gene-based |
| Anktiva (N-803) | Immunotherapy | BCG-unresponsive CIS ± papillary tumors (with BCG) | Fatigue, flu-like symptoms, urinary urgency | FDA-approved with BCG; IL-15 superagonist; promising results in BCG-unresponsive disease |
| UGN-102 (mitomycin gel) | Chemotherapy | Low-grade intermediate-risk NMIBC | Urinary frequency, dysuria, hematuria, bladder spasms | Thermo-sensitive gel; prolongs drug contact time; promising in low-grade tumors |
| TAR-200 (gemcitabine implant) | Chemotherapy delivery system | BCG-unresponsive NMIBC | Urinary tract irritation, dysuria, urinary retention | Implant releasing gemcitabine over weeks; alternative delivery approach |
Regular cystoscopy, urine tests, and imaging to monitor for recurrence.
| Risk Category | Cystoscopy | Urine Cytology | Imaging (Upper Tract) | Other Notes |
|---|---|---|---|---|
| Low-Risk | Every 3 months for 6–12 months, then annually | Optional | Only if indicated (e.g., hematuria) | May stop after 5 years if no recurrence |
| Intermediate-Risk | Every 3 months for 2 years, every 6 months to 5 years, then annually | At each visit | Every 1–2 years or as needed | Consider single-dose intravesical chemo post-TURBT |
| High-Risk | Every 3 months for 2 years, every 6 months until year 5, then annually | At each visit | Annually (CT urogram or ultrasound + cytology) | Consider repeat TURBT, BCG maintenance, or early cystectomy |
| Risk Group | 1-Year Recurrence Risk | 5-Year Recurrence Risk | 1-Year Progression Risk | 5-Year Progression Risk | Common Characteristics |
|---|---|---|---|---|---|
| Low Risk | 15% | 31% | <1% | ~1% | Small, single, low-grade Ta tumor, no CIS |
| Intermediate Risk | 24–38% | 38–62% | 1–5% | 6–17% | Multiple or recurrent low-grade tumors, no CIS |
| High Risk | ~61% | ~78% | ~17% | >45% | High-grade T1, CIS, large/multiple tumors |
Whether you’re seeking expert care for a urological condition or looking for a second opinion, we’re here to support you every step of the way. Reach out to schedule an appointment, ask questions, or learn more about personalized, minimally invasive treatment options tailored to your needs.